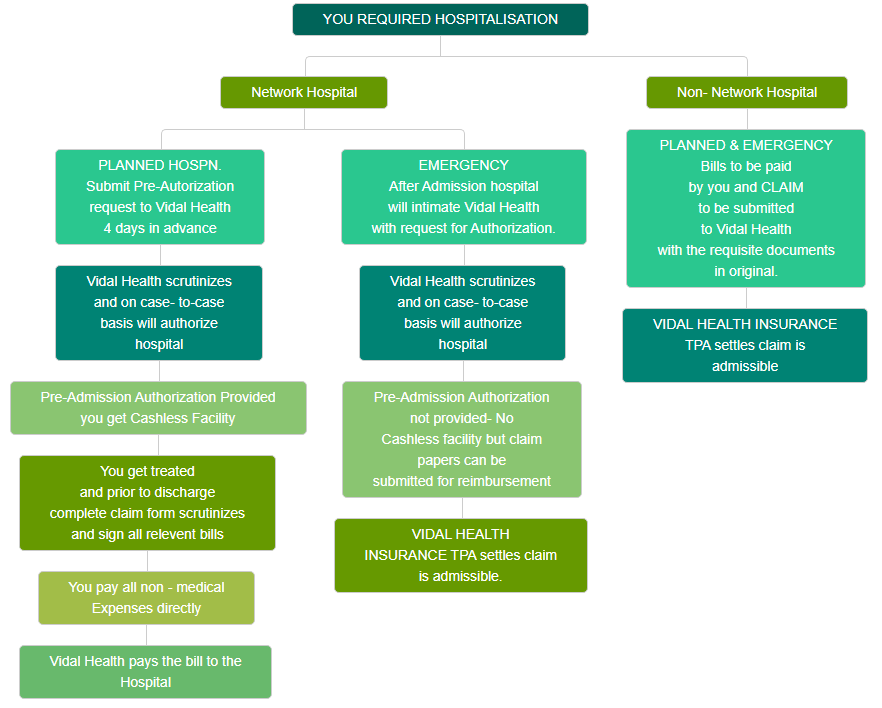
Process Flow Chart
Cashless Procedure
If you are planning hospitalisation
You need to do the following…
Fill the Pre - Authorisation Form, available with the Network Hospitals upon showing Vidal Health Card. This can also be obtained from any of the Vidal Health Insurance TPA Pvt. Ltd. branch offices or can be downloaded from this site.
- Submit / Fax the Pre-Authorisation Form at our local branch office 4 days in advance.
- If your hospitalisation is authorised, then ensure:
- You pay for non-medical expenses and
- Sign the relevant documents including a claim form before leaving the hospital / getting discharged.
- If your hospitalisation is rejected, then you can then submit a claim for reimbursement purpose at the Vidal Health Insurance TPA Pvt. Ltd. Branch office near you. (See Claims Settlement Procedure).
REMEMBER! - Vidal Health Insurance TPA Health Card issued to you is NOT a Credit Card, it is just complementary to your Mediclaim policy, and only on verification of your coverage, will you be given CASHLESS treatment Your cashless treatment will begin at the hospital, only after the hospital receives Authorisation confirming the same.
When you need emergency hospitalisation
Please follow the guidelines and update your family members so they would know what to do:
- Get admitted into a network immediately.
- Please inform your family member / relative to contact the billing dept in the hospital to inform them to intimate Vidal Health Insurance TPA Pvt. Ltd.
- If your hospitalisation is authorised, then ensure:
- You pay for non-medical expenses and
- Sign the relevant documents before leaving the hospital / getting discharged.
- If your hospitalisation is rejected, your treatment will be continued at the hospital. After discharge, you can then submit a claim for reimbursement purpose at the Vidal Health Insurance TPA Pvt. Ltd. Branch office near you. (See Claims Settlement Procedure).
- YOU REQUIRED HOSPITALISATION
Claim Settlement Procedures
To settle your claims, it is essential that every policy holder go through a 3 step cycle which is called.
(1) Claim Intimation / Notification (2) Claim document procurement and (3) Claim submission.
(1) Claim Intimation / Notification
Under Mediclaim, in case of hospitalisation, the policy holder should primarily ensure that the Vidal Health Insurance TPA Pvt. Ltd. is informed within 7 days of the hospitalisation. This preliminary notice should be submitted to Vidal Health Insurance TPA Pvt. Ltd. prior to the claim and the same should contain the following particulars:
- Vidal Health / TTK HTPA Card Number or Policy Number.
- Certificate Number.
- Nature of illness and / or injury.
- Name and address of the attending physician.
- Name of the hospital or nursing home, attending doctor.
- Bed number in the hospital.
(2) Claim Document Procurement
- Hospital Bill with Receipt for payment along with the break up signed by the policy holder.
- In case of surgeons / consultants bills, kindly insist on a stamped, preferably numbered receipt, Doctor's prescription and medicine bills.
- Discharge summary sheet from the hospital.
- Pathological reports and other investigation reports along with the doctor's authorization.
- Other relevant details and documents connected to hospitalisation.
(3) Claim submission
All the above need to be enclosed along with the Claim Form that can be obtained from the nearest Vidal Health Insurance TPA Pvt. Ltd. office or can be download by clicking on the downloads in left menu.
This claim form must be filled fully and sent to the nearest Vidal Health Insurance TPA Pvt. Ltd. office along with the following documents in original.
Note: Only expenses related to hospitalisation will be reimbursed as per the policy taken. All non-medical expenses will not be reimbursed.

